Third Party Adminstrator Leverages Automation to Deliver for Member Organizations
Employers are increasingly turning to Third Party Administrators (TPAs) to rein in rising healthcare costs and help improve employee health. Processing medical insurance and prescription claims, determining eligibility, managing plans, expenses and wellness programs have traditionally been very resource-intensive processes.
Transformational change was made possible by leveraging PilotFish’s integration engine solution. Automating these processes and making strategic use of data and analytics allowed this leading TPA to improve customer service, deliver value and design sustainable benefit plans to its booming employer client base.
THE CLIENT
The client is a full-service Third Party Administrator (TPA) that develops sustainable employee benefit plans designed to decrease healthcare costs and improve employee health for its member organizations. The client offers employers a suite of benefit administrative services and predictive analytics. Their services include medical plan management and reconciling employer members’ enrollment information against insurance carrier data.
THE CHALLENGE
The client’s growth was being stymied by a resource-intensive and highly manual process combined with a tight labor market. In order to scale up for growth and meet member demand, this TPA had to implement transformational changes in its processes and leverage emerging technology.
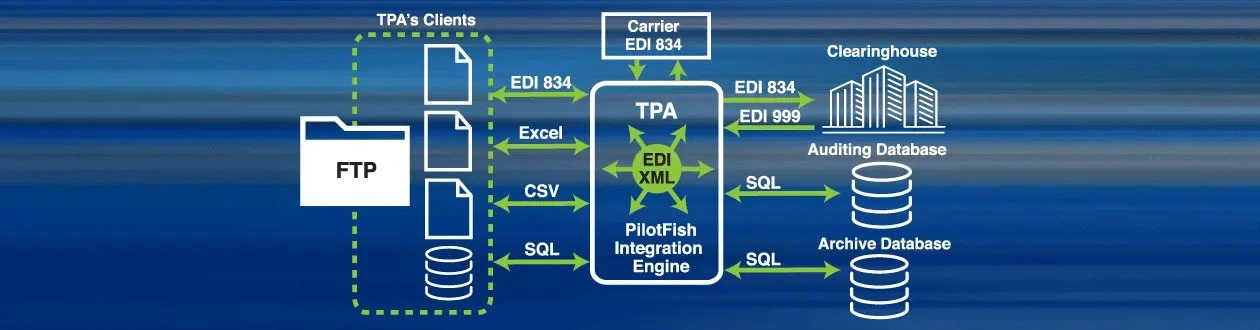
The client’s data exchange requires extensive use of HIPAA EDI transaction sets. Particularly challenging were EDI 834 benefit enrollment and maintenance, EDI 837 claims transactions and NCPDP. Each of these national TPA’s customers (new and existing) required rapid integration while also ensuring that the data quality was there. With a large and growing client base, high volumes of EDI data of widely differing quality and a multitude of other formats (CSV, PDFs, Excel, etc.) arrived daily. Each of these data formats requires efficient and accurate processing.
The 834 Inbound and Outbound processes take enrollment information from the TPA’s clients and reconcile that information against what the insurers have on their side. The results are returned to their clients via 834 EDI, CSV and whatever format the client requires.
The TPA’s previous process consisted of one-off interfaces. Its scarce technical resources were being used to write custom code and map each client’s interfaces, which was both time-consuming and difficult to maintain. The process was not sustainable nor was it scalable. The urgent business requirement was to automate the manual processes and validate the data to achieve 100% quality checks. What they needed was faster implementations and deployments while simultaneously providing higher quality at a lower cost.
What they also needed was a technology solution that offered a quick learning curve – so that in-house resources could become self-sufficient and their reliance on outside consultants could be minimized.
THE SOLUTION
The TPA selected PilotFish as its technology partner. PilotFish had built its reputation on “Anything to Anything” integration. With 24 years of experience in the insurance industry and an architecture designed to support working with any data format and communications protocol, PilotFish had a proven record of success. Likewise, its graphical automated interface assembly line process for interface configuration, management and maintenance had long offered organizations a path to becoming self-sufficient. With the adoption of PilotFish, all of this TPA client’s objectives could be met.
With PilotFish’s eiConsole for X12 EDI, EDI transactions are all parsed and mapped simply and quickly – regardless of format and source. The PilotFish integration engine’s built-in capabilities for incoming data translation, outgoing transaction construction, acknowledgment generation, process orchestration and scheduling met all of the client’s workflow and technical requirements.
The eiConsole delivered features and modules that stripped away the technical complexity of parsing, validating, mapping and producing all HIPAA EDI files. In this case, it streamlined and automated the handling and processing of member EDI 834 Enrollment and Maintenance data at scale. This was done while also meeting the company’s goals to inaugurate 100% consistency and error checking – all first priorities set for the eiConsole.
PilotFish’s Graphical Automated Interface Assembly Line process and visual drag & drop Data Mapper quickly negated the company’s need for custom coding and scripting, thus saving the client time and money. As every configuration followed the product’s intuitive user interface and consistent methodology, the client’s business users would be able to easily handle up to 90% of the work – freeing up their higher-level IT talent as well as further reducing their costs.
Preprocessing and validation are simple matters with the eiConsole. Built-in functionality was easily invoked and set for EDI or other data to be cleared to enter the processing stage and system. PilotFish was able to identify submission errors immediately and prevent processing delays. Automating error and consistency checking of incoming and outgoing data via PilotFish’s eiConsole met the client’s priority goal to move expeditiously to 100% checking and reporting of incomplete and incorrect data. Reporting of data anomalies and inaccuracies to each one of the vendors that the TPA worked with immediately improved data quality and accuracy of member (and other) information exchanged. This was both a cost-savings and a boost to customer satisfaction.
THE BENEFITS
Faster implementations and deployments were achieved. Working hand in hand with the PilotFish professional services team, the client was able to achieve faster implementation times and rapid deployment. The speed and efficiency validated the selection team’s decision that PilotFish would optimize both financial and IT resources early in its adoption.
Throughout each stage – PilotFish’s expertise, experience and unparalleled success rate in integration allowed this large national TPA to avoid the common pitfalls in dealing with HIPAA EDI 834s and other data exchanges. Onboarding of new customers became seamless, fast and pain-free. Customer satisfaction was greatly improved and earlier revenue capture was realized, thus providing this TPA with a formula for scalability and financial success.
Since its founding in 2001, PilotFish has been solely focused on the development of software products that enable the integration of systems, applications, equipment and devices. Billions of bits of data transverse through PilotFish software connecting virtually every kind of entity in healthcare, 90% of the top insurers, financial service companies, a wide range of manufacturers, as well as governments and their agencies. PilotFish distributes Product Licenses and delivers services directly to end users, solution providers and Value-Added Resellers across multiple industries to address a broad spectrum of integration requirements.
PilotFish will reduce your upfront investment, deliver more value and generate a higher ROI. Give us a call at 860 632 9900 or click the button.
X12, chartered by the American National Standards Institute for more than 35 years, develops and maintains EDI standards and XML schemas.