Proven EDI Claims Processing for Property & Casualty Insurers
and Health Payers
Processing and working with EDI claims poses many challenges for Property & Casualty Insurers and Health Payers. X12 EDI has a complex data structure and each EDI message, such as healthcare claims contain intricate data structures with numerous data elements and codes. The EDI 837 transaction set can include hundreds of data elements. ICD-10 diagnosis and procedure codes consist of tens of thousands of individual codes and descriptors. Healthcare claims processing typically involves hundreds to thousands of data elements and codes.
Mapping these data structures to the appropriate EDI format (such as X12) can be complex and time-consuming. Mapping requires the careful handling of data elements, segments and loops. Inconsistent or incorrect mapping can lead to data errors or rejection of claims. Another challenge is validating the accuracy, completeness and consistency of claims data required for successful processing. Payers must comply with Industry Standards such as HIPAA, X12 or other regional regulatory frameworks. The right EDI solution is essential for achieving efficiency, accuracy and compliance in your claims management or health claims processes.
PilotFish eiSuite – The Best-in-Class X12 EDI Integration Platform
PilotFish offers the best-in-class EDI integration platform designed specifically for insurers and payers. With our robust EDI solution, you can achieve unparalleled efficiency, accuracy and compliance.
Our robust data transformation and mapping tools seamlessly convert your internal claims data to the required EDI format, facilitating accurate and compliant data exchange. With PilotFish you can handle EDI message complexities, eliminating worries over complex mapping challenges and data errors often leading to claim rejections or delays.
With PilotFish, you can effortlessly handle the complexities of healthcare claims, including intricate data structures, hundreds of data elements and thousands of codes. Our EDI data integration platform provides comprehensive validation, error handling and compliance with industry standards like HIPAA, upholding the integrity and security of your claims data.
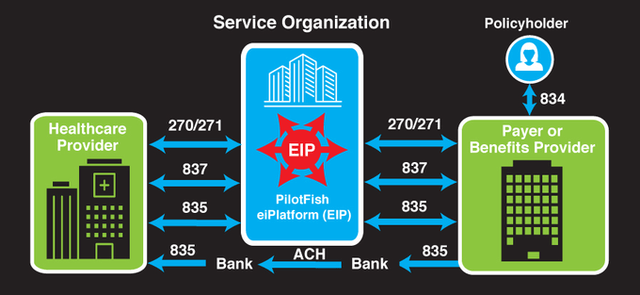
Experience streamlined workflows with real-time processing and automation, thus reducing manual effort and accelerating your claims management. PilotFish also supports seamless connectivity and communication with healthcare providers and intermediaries, enabling smooth EDI message data exchanges and timely claims adjudication.
Gain valuable insights into your claims operations through PilotFish’s advanced reporting and analytics features. Track key performance indicators, identify trends and make data-driven decisions to improve your business processes continuously.
Join leading insurers and payers who trust PilotFish’s insurance EDI integration platform to optimize their claims management and health claims processes. Make PilotFish your data integration platform and experience a new efficiency, accuracy and compliance level.
The PilotFish eiSuite provides a comprehensive solution for claims processing. The eiSuite consists of 4 complimentary offerings:
- eiPlatform – the Java runtime component for unattended execution of your interfaces
- eiConsole for X12 EDI – the IDE and the developer’s workstation for configuring, managing and maintaining interfaces
- eiDashboard – a web-based application for interface monitoring and reporting
- eiSuite EDI SNIP4+ – a complete solution suite for X12 EDI integration that supports all X12 transactions, SNIP 1-7 with validation and an optional add-on Code Set Maintenance subscription for updating and maintaining external code sets
Now let’s look in detail at the features and capabilities offered in the PilotFish eiSuite that streamline data exchange and automate claims handling.
EDI Standard Support & Compliance
Regarding standards support and compliance in claims management and health claims processing, PilotFish stands out as a leading insurance EDI integration platform solution. With robust support for various data formats and standards, including the widely used X12 standard, PilotFish’s integration platform empowers insurers and payers to seamlessly process and transform claims-related data while adhering to industry standards. By providing comprehensive compliance validation capabilities, PilotFish ensures accurate and complete validation of incoming claims or enrollment data, safeguarding compliance with X12 standards and regulatory requirements. With PilotFish, insurers and payers can be confident knowing that their claims management processes align with industry standards and regulatory guidelines.
- X12 Standards Support: PilotFish provides robust support for various data formats and standards, including X12. PilotFish’s integration platform has built-in capabilities to parse, validate and generate X12 messages such as EDI 837, EDI 834, EDI 835 and EDI 270/EDI 271. This capability allows for the seamless processing and transformation of claims-related data following industry standards.
- Compliance Validation: PilotFish provides comprehensive validation capabilities to enforce compliance with X12 standards and regulatory requirements. The solution includes pre-built validation rulesets specific to X12 transaction sets, enabling insurers or payers to validate incoming claims or enrollment data for accuracy, completeness and adherence to regulatory guidelines.
EDI Data Mapping & Transformation
PilotFish’s robust data mapping capabilities give insurers and payers a significant advantage in their claims processing operations. With a user-friendly interface and flexible data mapping rules, PilotFish empowers insurers and payers to seamlessly transform and map data elements between internal and the X12 EDI formats. PilotFish’s exclusive 3-pane data mapper allows for intuitive visual drag & drop mapping, thus enabling precise specification of transformations, conversions and value lookups.
The PilotFish solution offers an EDI parser that supports the parsing, mapping and translating of various code sets and terminologies commonly used in insurance EDI claims automation. This ensures accurate conversion between proprietary and standard code sets. With the ability to handle hierarchical data structures, enrich data from multiple sources and perform data validation and error handling, PilotFish empowers insurers and payers to achieve accurate, compliant and efficient claims processing.
- Flexible Data Mapping: PilotFish provides a user-friendly interface that enables insurers or payers to define and configure complex data mapping rules. These rules allow for the transformation and mapping of data elements between internal formats (proprietary formats or database structures) and the X12 EDI format (such as EDI 837 for claims). PilotFish’s exclusive 3-pane data mapper allows users to visually drag & drop map source data elements to their corresponding target X12 elements, specifying transformations, conversions or value lookups as needed.
- Built-in Transformation Functions: PilotFish’s Data Mapper offers a comprehensive library via a palette of XSLT transformation features and functions, including mathematical calculations, string manipulation, date formatting, conditional logic and more. These functions can be applied within the data mapping rules to transform and manipulate the data during the mapping process. This flexibility allows insurers or payers to handle complex data transformations and ensure accurate conversion between internal formats and X12 standards.
- Support for Code Sets and Terminologies: PilotFish’s Data Mapper supports the mapping and translation of various code sets and terminologies commonly used in healthcare claims processing. This includes mapping between internal code sets (such as a proprietary procedure or diagnosis codes) and standard code sets like ICD-10 diagnosis and procedure codes, CPT codes or HCPCS codes. The solution allows seamless conversion and mapping of these codes to comply with X12 standards and ensure accurate claims processing.
- Hierarchical Data Mapping: Hierarchical data structures may exist in claims processing, such as multiple service lines associated with a claim or nested data elements within a claim. PilotFish’s solution supports the mapping and transformation of such hierarchical data, enabling insurers or payers to accurately represent and convert complex data structures to the corresponding X12 hierarchical segments, loops and subloops.
- Data Enrichment and Augmentation: PilotFish provides capabilities to enrich and augment data during the transformation and mapping process. Insurers or payers can incorporate additional data from internal or external sources, such as lookups to provider directories, fee schedules or eligibility databases, to enhance the claims data before converting it to X12 EDI format. This ensures that the transformed data is comprehensive and meets the specific requirements of downstream systems or trading partners.
- Data Validation and Error Handling: PilotFish includes validation and error handling features within the data transformation and mapping process. Insurers or payers can define validation rules and data consistency checks during the mapping, ensuring that the transformed data meets the required standards and business rules. Any data errors or inconsistencies can be flagged and handled through the built-in error handling mechanisms, allowing for prompt resolution and promoting data accuracy in claims processing.
EDI Connectivity & Automation
PilotFish offers insurers and payers significant advantages in claims processing with its connectivity options and automation features. Seamlessly connect with healthcare providers through various protocols and automate workflows for efficient claims management. Proactive error handling and real-time notifications ensure prompt issue resolution. PilotFish facilitates streamlined operations, increased productivity and error-free claims processing with these features.
- Broad Connectivity Options: PilotFish supports multiple connectivity options, such as secure file transfer protocols (e.g., FTPS, SFTP), web services (e.g., SOAP, REST) or direct system-to-system integration via APIs. This flexibility allows insurers or payers to connect seamlessly with healthcare providers, clearinghouses or intermediaries for the exchange of EDI transactions related to claims management. (40+ Listeners)
- Workflow Automation: PilotFish offers workflow automation capabilities to streamline the claims management process. The solution usually includes features like automated routing, event triggers and exception handling, allowing for efficient claims processing, status tracking and escalation. This automation reduces manual effort, accelerates the overall process and improves productivity.
- Proactive Error Handling and Notifications: The PilotFish integration platform includes robust error-handling mechanisms, logging and notification features. It captures and reports any data or processing errors encountered during EDI integration, allowing insurers or payers to identify and resolve issues quickly. Users can set up Real-time alerts and notifications to ensure timely responses and minimize disruptions in the claims management process.
EDI Reporting, Compliance, and Scalability
With PilotFish, insurers and payers gain a competitive edge in reporting, compliance and scalability for their claims management. The solution offers powerful reporting and analytics capabilities, empowering users to gain valuable insights into claims management operations, monitor KPIs, track claim volumes and make data-driven decisions for process improvement.
Compliance is prioritized through robust security measures, including encryption protocols, secure data transmission and access controls, ensuring the protection of sensitive healthcare information and adherence to HIPAA regulations. PilotFish’s scalability and seamless integration support also enable insurers and payers to handle growing data volumes, achieve end-to-end automation and optimize their claims management processes.
- Reporting and Analytics: PilotFish offers reporting and analytics capabilities, providing insurers or payers valuable insights into their claims management operations. The solution offers customizable dashboards and reporting tools, enabling users to monitor key performance indicators (KPIs), track claim volumes, identify trends and make data-driven decisions for process improvement.
- Compliance and Security: PilotFish prioritizes compliance with industry standards, including data security and privacy regulations like HIPAA. PilotFish’s integration solution supports encryption protocols, secure data transmission and access controls to protect sensitive healthcare information during EDI integration. It also supports audit trails to maintain compliance with regulatory requirements.
- Scalability and Integration: PilotFish provides scalability and flexibility to accommodate growing data volumes and integration needs. It supports seamless integration with other internal systems, such as claims management or adjudication systems, enabling insurers or payers to achieve end-to-end automation and optimize the claims management process.
EDI Healthcare External Code Set Maintenance
PilotFish has a process for continuously updating the millions of X12 EDI codes including intricate procedures like claim auditing and claim scrubbing. Maintaining these can become very time-consuming, with tens of thousands of unique individual codes and descriptors for ICD-10 diagnosis and procedures and insurance healthcare claims with hundreds to thousands of data elements and codes. Some codes are updated annually, others semi-annually, quarterly, or irregularly. PilotFish offers an optional subscription for continuous updates and maintenance of EDI Healthcare External Code Sets to relieve customers of this burden. Through this service, PilotFish ensures seamless integration of crucial components like claim scrubbing or claim auditing into the code data files, which are made available via the EDI SNIP Validation Processor in the eiConsole. Customers receive timely notifications as these become available, ensuring their systems remain current and compliant.
PilotFish – The Proven EDI Integration Platform for Your Success
PilotFish software is utilized by 90% of the top insurers and leading health payers. Its proven EDI claims processing solutions for Property & Casualty insurers and Health Payers address the challenges associated with complex data structures, data mapping, validation, compliance and scalability. With a comprehensive suite of features and capabilities, PilotFish empowers insurers and payers to achieve efficiency, accuracy and compliance in their claims management or health claims processes.
The PilotFish solution supports X12 standards, provides robust data mapping and transformation tools, facilitates seamless connectivity and automation, offers powerful reporting and analytics capabilities, prioritizes compliance and security and ensures scalability and integration. Additionally, PilotFish’s optional code maintenance service relieves customers of the burden of code updates, ensuring continuous compliance with changing industry requirements. Choose PilotFish for unparalleled performance and success in your insurance healthcare claims management operations.
If you’re curious about the software features, free trial, or even a demo – we’re ready to answer any and all questions. Please call us at 860 632 9900 or click the button.
X12, chartered by the American National Standards Institute for more than 35 years, develops and maintains EDI standards and XML schemas.

